Peutz-Jeghers syndrome in Adult
See also in: Oral Mucosal LesionAlerts and Notices
Important News & Links
Synopsis

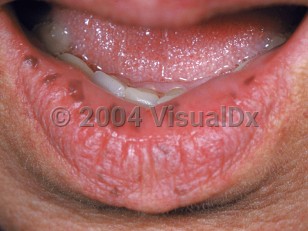
Peutz-Jeghers syndrome (PJS) is a rare autosomal dominant syndrome associated with both mucocutaneous pigmentation and multiple intestinal hamartomatous polyps. The genetic defect is due to mutations in serine / threonine kinase 11 (STK11) gene.
Pigmented cutaneous and mucosal macules usually present at birth or in infancy. Those on the skin and lips fade around the time of puberty but the intraoral macules tend to persist. The gastrointestinal (GI) polyps typically present in adolescence or early adulthood and are most commonly in the small intestine, although any part of the GI tract may be involved. Polyps may also be extraintestinal, such as in the respiratory and urinary tracts.
Patients with polyps in the GI tract may present with abdominal pain, GI bleeding, diarrhea, intussusception, or obstruction. The polyps are benign hamartomas. They may start to grow early in childhood, but tend to develop in the second decade.
Because STK11 is a tumor suppressor gene, patients with PJS have an increased risk of developing malignant tumors compared with the general population. In a 2010 systematic review looking at over 1000 PJS patients, colorectal cancer was the most common malignancy, followed by breast, small bowel, gastric, and pancreatic cancer. Testicular and ovarian cancer risk is also increased. The GI tract polyps themselves have a cumulative risk of around 13% of developing into small intestine carcinoma. Malignancies typically arise in adulthood (for example, the mean age of diagnosis for small intestine cancer is 42 years), so patients should undergo frequent cancer screenings.
Pigmented cutaneous and mucosal macules usually present at birth or in infancy. Those on the skin and lips fade around the time of puberty but the intraoral macules tend to persist. The gastrointestinal (GI) polyps typically present in adolescence or early adulthood and are most commonly in the small intestine, although any part of the GI tract may be involved. Polyps may also be extraintestinal, such as in the respiratory and urinary tracts.
Patients with polyps in the GI tract may present with abdominal pain, GI bleeding, diarrhea, intussusception, or obstruction. The polyps are benign hamartomas. They may start to grow early in childhood, but tend to develop in the second decade.
Because STK11 is a tumor suppressor gene, patients with PJS have an increased risk of developing malignant tumors compared with the general population. In a 2010 systematic review looking at over 1000 PJS patients, colorectal cancer was the most common malignancy, followed by breast, small bowel, gastric, and pancreatic cancer. Testicular and ovarian cancer risk is also increased. The GI tract polyps themselves have a cumulative risk of around 13% of developing into small intestine carcinoma. Malignancies typically arise in adulthood (for example, the mean age of diagnosis for small intestine cancer is 42 years), so patients should undergo frequent cancer screenings.
Codes
ICD10CM:
Q85.89 – Other phakomatoses, not elsewhere classified
SNOMEDCT:
54411001 – Peutz-Jeghers syndrome
Q85.89 – Other phakomatoses, not elsewhere classified
SNOMEDCT:
54411001 – Peutz-Jeghers syndrome
Look For
Subscription Required
Diagnostic Pearls
Subscription Required
Differential Diagnosis & Pitfalls

To perform a comparison, select diagnoses from the classic differential
Subscription Required
Best Tests
Subscription Required
Management Pearls
Subscription Required
Therapy
Subscription Required
References
Subscription Required
Last Reviewed:06/20/2019
Last Updated:02/29/2024
Last Updated:02/29/2024
Peutz-Jeghers syndrome in Adult
See also in: Oral Mucosal Lesion